Top 5 Medical Billing Mistakes Clinics Still Make in 2025 — And How I Help Fix Them
Despite all the advancements in healthcare tech, some things haven’t changed — clinics are still losing revenue due to the same avoidable medical billing mistakes.
As a freelance medical billing specialist, I’ve seen it all — the overworked front desk, the outdated workflows, the denials piling up. The good news? Most of these issues are 100% fixable.
Here are the top five medical billing mistakes I still see in 2025 — and how I help clinics like yours solve them before they turn into lost revenue.
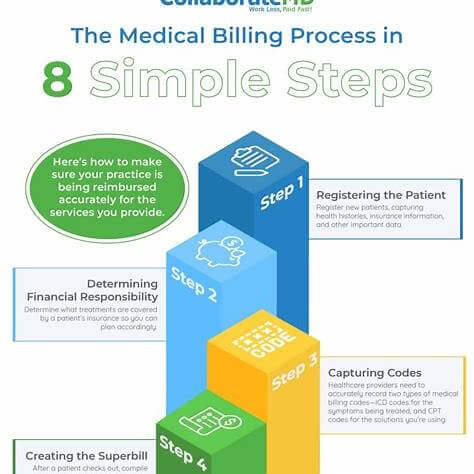
1. Incomplete or Inaccurate Patient Information
“We didn’t know their insurance changed.”
Sound familiar? Missing or outdated insurance details is one of the most common reasons claims get denied — and it’s still happening every day.
How I fix it:
I help clinics implement front-end checks and eligibility verification tools that flag issues before the claim is even created. I also train staff on what to watch for — because sometimes it’s as simple as a typo.
✅ Result: Fewer denials, faster payments.
2. Coding Errors and Outdated Codes
“We thought that CPT code was still valid.”
With 2025’s updated coding guidelines and increasing payer scrutiny, mistakes in coding cost clinics thousands in rejections, delays, or underpayments.
How I fix it:
I stay updated on ICD-10, CPT, and payer-specific code changes so you don’t have to. I also audit claims regularly to catch errors before they go out the door.
✅ Result: Clean claims, higher reimbursement, fewer resubmissions.
3. Late or Missed Claim Submissions
“We didn’t realize the claim deadline passed.”
Yes, even in 2025, practices are missing deadlines — and losing out on money they’ve already earned. Most payers have short windows (as little as 90 days!) for claim submission.
How I fix it:
I use smart tracking systems and workflows that flag pending or aging claims automatically. I make sure your claims are submitted on time, every time.
✅ Result: No more leaving money on the table.
4. Weak Denial Management Processes
“We’ll get to those denials eventually…”
Denials can easily get buried under the day-to-day chaos. But ignoring them is like ignoring a leaky faucet — it gets expensive fast.
How I fix it:
I create a custom denial follow-up system that tracks each claim, categorizes denials, and submits well-documented appeals quickly. I also provide monthly reports so you know where things stand.
✅ Result: More overturned denials. Better cash flow. Less stress.
5. Poor Communication Between Clinical and Billing Teams
“The doctor thought they documented it…”
Billing can’t do its job if documentation is missing or unclear. And in small clinics, there’s often a communication gap between front desk, provider, and billing.
How I fix it:
I act as a bridge between clinical and admin staff. I review charts for billing gaps, flag documentation issues, and even provide mini-training sessions to keep everyone aligned.
✅ Result: Cleaner documentation. Smoother billing. Happier staff.
💬 Final Thoughts: You Don’t Have to Do It Alone
Running a clinic in 2025 is no joke — between regulatory changes, rising patient expectations, and tighter payer rules, it’s a lot to juggle.
That’s where I come in.
As a freelancer, I offer clinics a flexible, hands-on approach to revenue cycle management. Whether you’re drowning in denials or just want to tighten up your process, I can help you get paid faster, reduce errors, and free up your team to focus on what matters most: patient care.
👉 Want to chat about how I can support your billing process? Drop me a message. No pressure, just a real conversation.
#MedicalBilling2025 #RevenueCycleManagement #FreelanceRCM #HealthcareBilling #ClinicManagement #MedicalBillingMistakes #HealthAdminTips
